World 1-3: How Does a Ventilator Work?
/Hello, SuperCaptainBraveFAM!
I’m Nurse Leah and I’m here with another installment of the Science Saga of SuperCaptainBraveMan!
In World 1-1, we learned about the lungs and what they do. We even made our own “mini-lung” to show how the lungs inflate inside the chest.
In World 1-2, we found out that CPR (aka: cardiopulmonary respiration) can be done using only our hands to pump blood through the body and bring the oxygen we need to where it has to go. At least, until experienced medical help can arrive!
Now we enter World 1-3. And I’d like to share with you one of the mechanical ways medicine can help support our lungs and provide precious oxygen to our body.
Before we continue, just a quick recap of the parts of the respiratory system. (Remember that’s the name of the body system that’s responsible for breathing!)
The mouth & nose help air go into and out of your body.
The trachea (aka the Windpipe) is the tube that connects the mouth & nose to your lungs.
The muscles in between your ribs and a large muscle called the diaphragm work together to increase the space inside the chest and cause the lungs to expand.
The lungs are protected in your ribcage and hold smaller, balloon-like structures called alveoli. These alveoli are where carbon dioxide and other waste gases are exchanged for fresh oxygen.
Oxygen is needed to create energy in every single cell in your body!
All these parts work together for the main purpose of getting rid of waste gases and gaining new oxygen.
Recap done; I just need to explain one extra science fact about breathing.
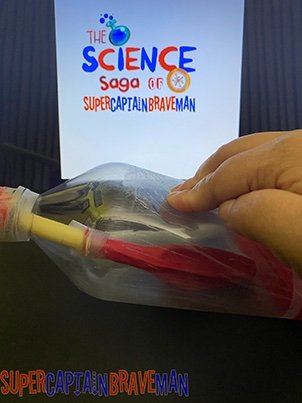
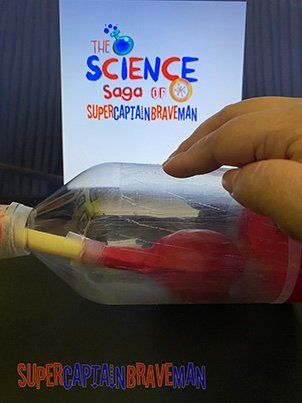
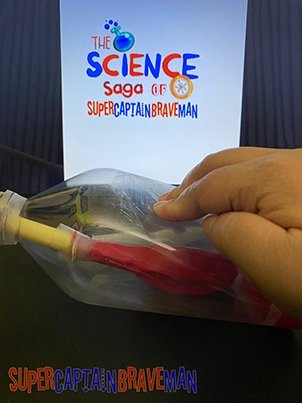
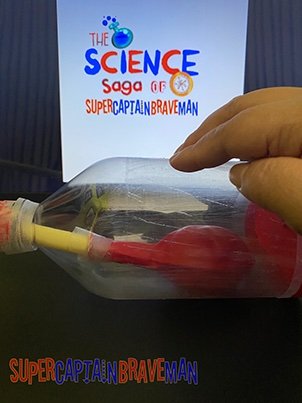
Look at our mini-lung!
If you still have the mini-lung from World 1-1, it’s a great visual example of what I’m talking about. When we made our mini-lung, we sealed off the bottom and top of the bottle. The balloon and straw inside the bottle now exist in a partial vacuum.
A vacuum is a space with nothing in it—not even air. A partial vacuum can have a little air or other stuff in it. The way scientists measure the strength of a vacuum is by using a measurement called pressure.
Because of the partial vacuum in the bottle, there are only 2 ways air can go in or out of the balloon.
Changing the shape and size of the bottle by pulling the stretched “diaphragm” or compressing the bottle sides.
Forcing air into the balloon by blowing directly through the straw.
The physical way our bodies take in air is option number 1; through a process called negative pressure breathing.
Since the space around the balloon is in a partial vacuum, this space will always want to have the same amount of pressure in it. By expanding the shape and size of the bottle, the pressure change inside will pull air in through the straw and inflate the balloon. The bigger the balloon gets, the closer to the original pressure the bottle becomes.
Air is pretty invisible so it may be hard to visualize how this works using just our mini-lung. If you have a medicine dropper, bulb syringe, or turkey baster, here’s a quick example of negative pressure in action.
Take your medicine dropper or turkey baster, squeeze the bulb a bit, put the tip in a cup of liquid, and let go of the bulb.
Where did the liquid go? Into the dropper!
That’s because items like medicine droppers, eye droppers, turkey basters, or those bulb syringes you use to suck up baby boogers all have partial vacuums!
Now, you might be thinking, “If negative pressure breathing exists, then positive pressure breathing is a thing too, right?”
You are absolutely correct!
Conventional CPR used by those trained in it, requires rescue breaths aka mouth-to-mouth. This is where air is blown into the lungs by an outside force.
The outside force can be the breath of a rescuer; air pushed through a large, self-inflating bag aka a bag valve mask; or in very serious and extended instances, a machine called a ventilator.
A ventilator is a form of life support. The machine takes over the work of breathing when a person isn’t able to breathe enough on their own. The ventilator pushes a mixture of air and oxygen into the lungs.
Very often, when someone has to use a ventilator, they also need extra oxygen. Using either oxygen tanks or an oxygen concentrator, tubes connect the source of the oxygen to the ventilator and into the person’s lungs.
Why would a person require extra oxygen if breathing normally already gives us all we need?
Imagine a handful of ice cream sprinkles—the rainbow kind. Some are white, some are pink, a few may be blue or light green. In a way, the air around us is a lot like that handful of sprinkles. Some of the air is oxygen, some is carbon dioxide, some is a gas called nitrogen or any other kind of gases. But altogether these separate gases make up the air we breathe.
Usually, breathing is enough. Our bodies sort through the different gases in the air and take the oxygen in as fast as it takes to take a breath. But, when a person isn’t able to breathe on their own, extra help is just that.
Extra help.
There are several reasons why a person would need a ventilator. One of the most common is because the help a ventilator gives allows the body to focus energy on other things like healing after an accident or during a severe infection.
Everything our bodies do require energy. Life support machines like ventilators help ease the strain on our bodies during the healing process.
In hospital settings like an ICU (intensive care unit), those using ventilators can have something called an endotracheal tube that connects the ventilator to them. This tube goes through the nose or mouth and into the Windpipe. And with the tube in place, they can’t talk or eat until it's removed.
Endotracheal tubes aren’t permanent and are removed when the person doesn’t need a ventilator anymore.
There are times when an endotracheal tube isn’t enough, though. If something is blocking the windpipe or the ventilator will be used for a long time, a tracheostomy procedure is performed.
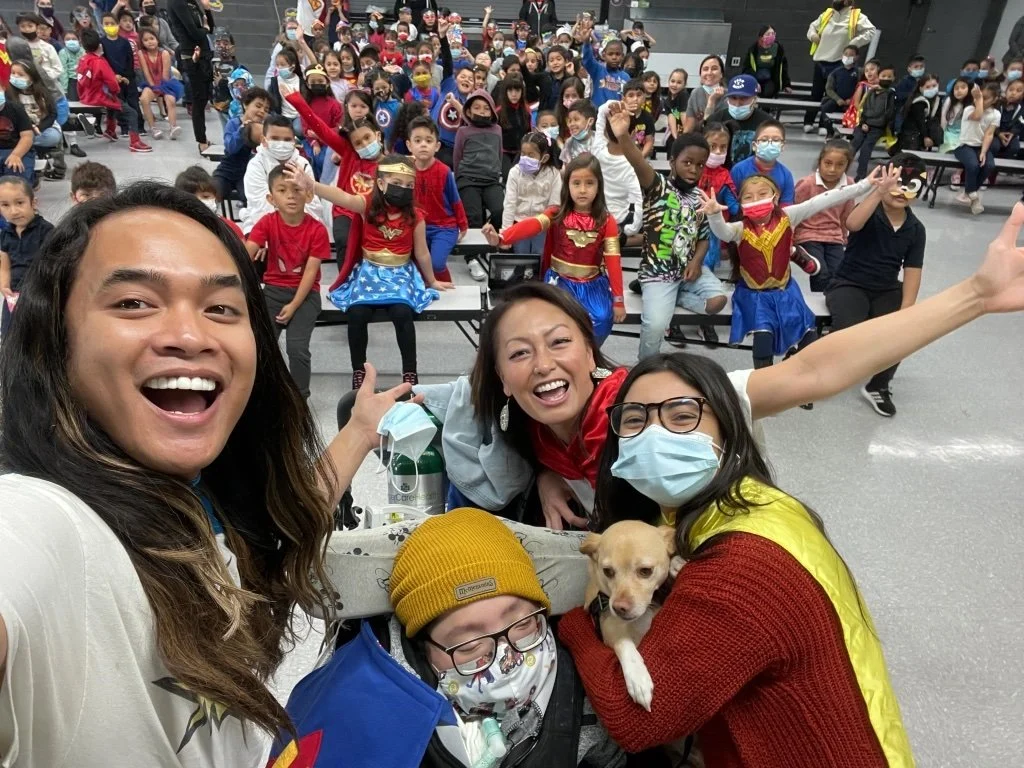
Kyle has a tracheostomy tube put in place by his doctors.
Kyle has a tracheostomy tube put in place by his doctors.
A surgeon creates a hole in the person’s neck & trachea and inserts a tracheostomy tube into the hole. That tube is then connected to the ventilator and the person now has a working airway. While the tracheostomy tube is in place, the person can still talk and eat as long as they're very careful.
Like the endotracheal tube, the tracheostomy tube—more commonly known as a trach—isn’t permanent and can be removed once the ventilator isn’t needed anymore.
Nurse Ashley checks Kyle's lungs before they begin the "sprinting" exercise.
When a person is getting better and the time comes to remove the ventilator, healthcare professionals will help them get used to breathing without it. Through a series of exercises and observational tests, healthcare workers assess a person’s ability to breathe on their own.
Nurse Ashley checks Kyle’s lungs before they begin the “sprinting” exercise.
For those with trachs, an exercise called “sprinting” is used. After disconnecting the ventilator tube, a small cap is placed over the trach. The person then focuses on breathing as normally as possible through their nose and mouth. After using a ventilator, the muscles used in respiration might need to retrain themselves for a bit.
Healthcare workers monitor the person closely and when the chosen sprinting time is reached, the ventilator is reconnected to the trach and the exercise is over. This is done again and for longer intervals until doctors believe that the person can breathe well on their own.
Breathing is an amazingly simple thing we do every day. Our bodies are designed so well that its something that happens naturally and mostly without conscious thought. So, when problems occur that mess with that function, scientists and doctors over the years have had to figure out new ways for people to breathe.
Science helped us discover how we breathe and is constantly searching to improve our knowledge in order to help others.
This adventure is far from over. Be sure to come back and explore new worlds with me in…
Until next week, stay safe and stay brave, SuperCaptainBraveFAM!
Join our mailing list and don’t forget to like & follow SuperCaptainBraveMan on social media for new posts and exciting news!
Instagram: @supercaptainbraveman
Facebook: www.facebook.com/supercaptainbraveman